I. Introduction
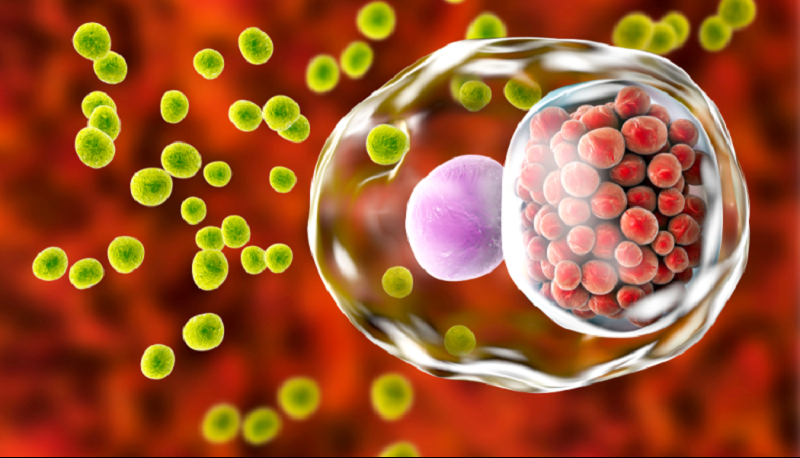
Chlamydia is a sexually transmitted infectious disease caused by the bacterium Chlamydia trachomatis. In the United States, it is the most commonly reported bacterial infection. Globally, it is the most common sexually transmitted infection. It causes an ocular infection called “trachoma,” which is the leading infectious cause of blindness worldwide.
In females, the cervix is the anatomic site that is most commonly infected. This can manifest as cervicitis, urethritis, pelvic inflammatory disease, perihepatitis, or proctitis. Chlamydial infections in women, especially if untreated, increase the risk of infertility and ectopic pregnancy, leading to high medical costs. There are also risks if a woman has an infection during pregnancy. Additionally, infants born vaginally to mothers infected with genital Chlamydia trachomatis may develop conjunctivitis and/or pneumonia.
In men, infection with Chlamydia trachomatis can lead to urethritis, epididymitis, prostatitis, proctitis, or reactive arthritis. Both men and women infected with C. trachomatis may also experience conjunctivitis, pharyngitis, and lymphogranuloma venereum. Lymphogranuloma venereum (LGV), caused by distinct serovars of Chlamydia trachomatis, is a less common disease characterized by enlarged lymph nodes or severe proctocolitis.
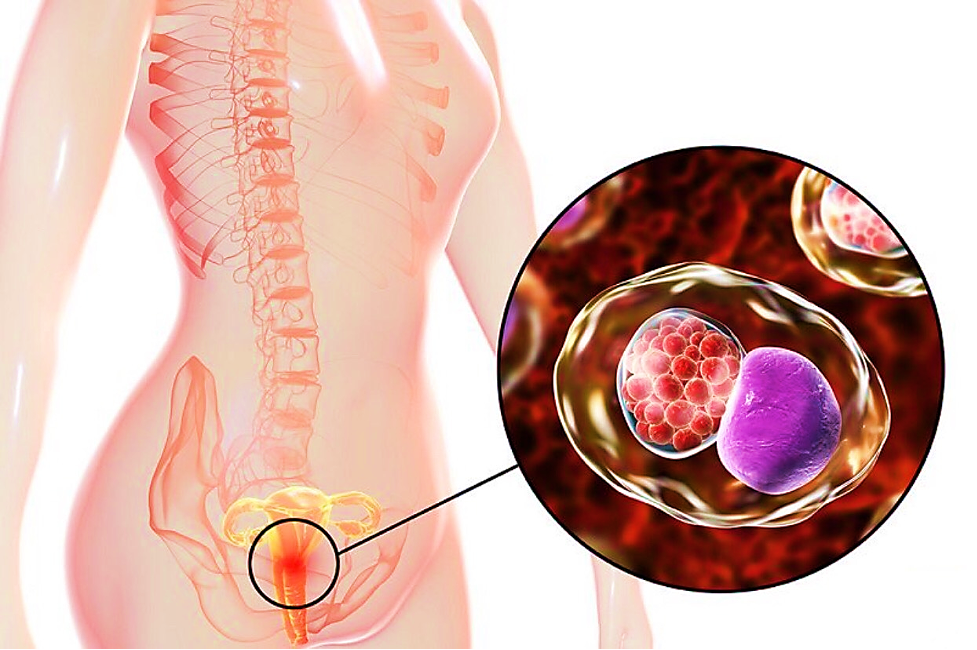
Hình 1. Chlamydia is a common sexually transmitted disease caused by bacteria called Chlamydia trachomatis
II. Epidemiology
Urogenital chlamydia infections are the most commonly reported bacterial infections in the U.S and the most common cause of sexually transmitted infections in the world. The overall rate of urogenital infection amongst U.S. women is two times that of U.S. men, with a higher prevalence in women 15-24 years of age and a higher incidence in men between 20-24 years of age.
III. Differential Diagnosis
Because Chlamydia trachomatis can lead to a broad spectrum of clinical diseases or manifestations, the differential diagnosis of various presenting complaints is also broad. One should consider other etiologies that may affect each body area or organ systems and may manifest similarly.
Dysuria:
-
Gonorrhea
-
Genital herpes
-
Urinary tract infection
Abdominal Pain:
-
Appendicitis
-
Cholecystitis
-
Constipation
Pelvic Pain:
-
Endometriosis
-
Ovarian cysts
-
Adenomyosis
Vaginal Discharge:
-
Bacterial vaginosis
-
Trichomonas vaginalis
-
Gonorrhea
-
Vaginal candidiasis
-
Foreign body
-
Mycoplasma genitalium infection
-
Ureaplasma infection
Rectal Discharge:
-
Inflammatory bowel disease
-
Gonorrhea
Conjunctivitis:
-
Viral infection
-
Allergy
-
Gonococcal infection
Postcoital or Intermenstrual Bleeding:
-
Cervical cancer
-
Cervical or endometrial polyp
-
Cervical ectropion
-
Leiomyoma
-
Pregnancy
Genital Ulceration:
-
Herpes simplex
-
Syphilis
-
Chancroid
-
Granuloma inguinale
IV. Treatment / Management
The goal of treatment is the prevention of complications associated with infection (e.g., PID, infertility), to decrease the risk of transmission, and the resolution of symptoms. Treatment for uncomplicated urogenital chlamydia infection is with azithromycin. Doxycycline is an alternative, but azithromycin is preferred as it is a single-dose therapy. Other alternatives include erythromycin, levofloxacin, and ofloxacin.
Chlamydial infection and gonococcal infections often coexist. In men, the co-treatment for urogenital gonococcal infection should occur on the basis of the detection of the organism on NAAT or gram stain. In women, the gram stain is less helpful due to the possibility of normal Neisseria species colonization within the vaginal flora. Therefore, co-treatment should be dependent on an assessment of individual patient risk and local prevalence rates.
Patients should have partners identified and tested. They should also be counseled on high-risk behaviors, avoid sexual activity for one week after initiating therapy, and should consider testing for HIV.
Verification of cure should occur three weeks after treatment completion, and retesting should be performed three months after treatment.
If symptoms persist after treatment, consider coinfection with a secondary bacterium or reinfection.
Nguồn:
https://www.ncbi.nlm.nih.gov/books/NBK537286/

 VI
VI